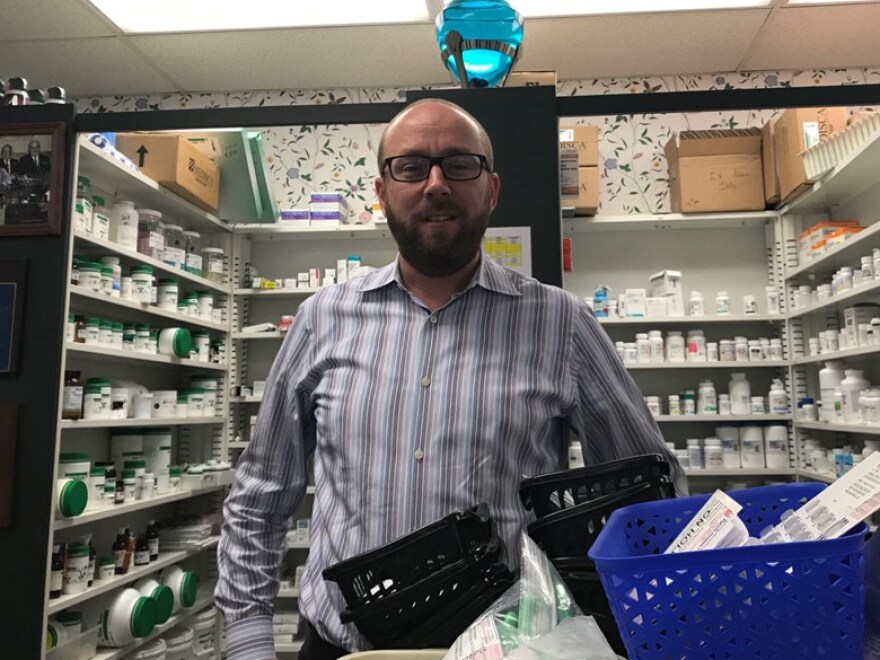
The floral wallpaper and cheerful signs at Pucci’s Pharmacy in Midtown Sacramento invoke an old-timey feel that sets it apart from a Rite Aid or CVS.
Behind the counter, owner Clint Hopkins greets the two resident support dogs, Allie and Ella, before counseling a patient about her inhaler.
Hopkins took over the 90-year-old pharmacy in 2016. Lately, he’s been struggling to make ends meet, because the state changed the way it reimburses him for buying certain prescription drugs. California is also taking back money from past claims, he said.
These challenges are spurring independent pharmacies across the state to question whether they can continue serving Medi-Cal patients.
“We’re stuck between a rock and a hard place, providing the medications to the patients that need them or being sorry we’re not filling prescriptions because we’re not being paid,” he said. “It’s only so long until it puts us out of business.”
In 2017, following a ruling from the federal government, the state Department of Health Care Services changed how it reimburses pharmacies that buy drugs for Medi-Cal patients. This applied only to patients in “fee-for-service” Medi-Cal, where the state pays the provider, in this case the pharmacy, directly for services rather than going through a managed care plan such as Anthem Blue Cross.
After California began implementing the new reimbursement rates in February, some pharmacies started getting less money back from the state when they submitted claims for these patients.
Now, these pharmacies say the lower rates are doing serious damage to their bottom lines.
Jon Roth of the California Pharmacists Association said small pharmacies that treat high numbers of chronically ill, low-income patients are being hit hardest.
“The issue really disproportionately affects what we call our independent community pharmacy, like ‘Joe’s drug store on main street,’” he said.
Hopkins said he’s losing money on patients with HIV, cancer and other complex conditions that require expensive medication. He’s committed to continuing to serve this population, but suspects other small pharmacies will stop ordering these drugs — or even shut their doors.
This spring, the California Pharmacists Association surveyed 241 independent pharmacies and found 85 percent have stopped serving Medi-Cal patients or are thinking about it, and 74 percent might close or sell their businesses.
The Department of Health Care Services says they reached the new reimbursement rates after several meetings with pharmacists across the state. They also decided to raise what’s called the “professional dispensing fee,” which the state pays to pharmacies for staffing and other operating costs.
Geoffrey Joyce, an associate professor with the University of Southern California’s School of Pharmacy, said this was an effort to standardize the variety of payments the state was making to pharmacies, and crack down on abuse in the Medicaid system.
“When I look at those reimbursing rates and dispensing fees, they’re very generous,” he said. “This is a step toward greater transparency.”
But it doesn’t shake out well for everyone. How the rate change affects a pharmacy depends on how big it is, how many patients it serves and what quantity of drugs it buys.
“It is an average, which means some pharmacies are going to get a price below that average and some are going to pay more,” he said. “And I’d imagine the smaller pharmacies, they may say, ‘Hey, you know what, we’re actually losing money on this spread.’”
On top of the shifted rates, the department recently started asking for money from some pharmacies.
For claims filed between 2017, when the new rates were approved, and when they actually took effect this February, the state was still reimbursing pharmacies at the old rate. Now, they’re telling pharmacies they should have been paid back at the new rate — and that they may owe the state the difference. Some pharmacies are getting money back from the readjustment.
The California Pharmacists Association is suing the department over this recoupment and also the new rates, so the take-back is on hold for now. The case is on the desk of federal judge in Oakland.
“Even though [independent pharmacies] are losing money on the go-forward, at least they don’t have the clawback on top of it,” Roth said. “But if the clawbacks come back into play … it’ll just be a matter of how quickly they go out of business, as opposed to whether they go out of business.”
Clint Hopkins had to give between $6,000 and $7,000 back to the state before the recoupment came to a halt.
“We’re waiting on that judgment,” he said. “We’re all on pins and needles.”
And he says the situation is a public health threat.
If independent pharmacies can’t stock vital medications, he argues more people will end up in the emergency room, and that the risk of infectious disease spread will increase.
“It is counterintuitive for the state to be expanding Medicaid coverage to more people, but simultaneously not ensuring that those enrollees have access to their necessary medications,” he said.
The Department of Health Care Services says it's assessing the impact to pharmacies and considering changes to the recoupment process. The CPhA says they’re trying to gain traction on the issue in the Legislature.
Copyright 2019 Capital Public Radio